New Clinical Study Highlights the Metabolic Factors of Hashimoto's Thyroiditis
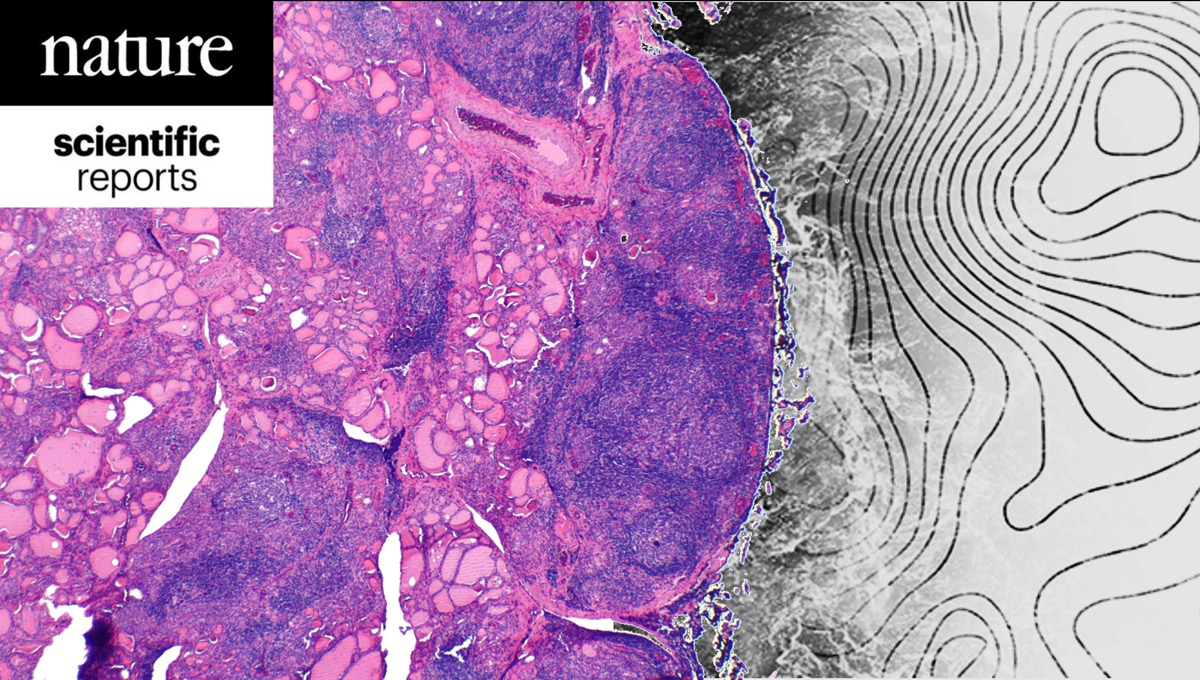
A new clinical study by our team, published in Nature Scientific Reports, sheds light on the metabolic causes of Hashimoto’s disease.
Hashimoto's thyroiditis, the most common autoimmune disease and leading cause of hypothyroidism, primarily affects women aged between 25 and 55.
Although hormone replacement therapy is the standard treatment, many patients continue experiencing symptoms such as fatigue, low energy levels, gastrointestinal issues, fluid retention, and weight management difficulties, despite having normal levels of TSH (Thyroid Stimulating Hormone). These persistent symptoms significantly impact patients' quality of life, highlighting the need to better understand and address the underlying causes of the disease.
The research was conducted by Metabolomic Medicine® and published in Nature Scientific Reports, the fifth most frequently cited scientific journal globally. It thoroughly explored the metabolic factors associated with Hashimoto's thyroiditis, emphasizing the roles of insulin resistance, inflammation, and gut microbiome balance.
The researchers found that insulin resistance, besides its strong connection to inflammation, may also limit the effectiveness of thyroid hormone treatment. Additionally, gut microbiome balance plays a crucial role. Dysbiosis (imbalance in intestinal flora) can worsen inflammation and disrupt thyroid hormone production, contributing to the overall decline in health.
Micronutrient Deficiencies & Thyroid Dysfunction
The study also identified low levels of essential micronutrients, such as iodine, iron, copper, chromium, selenium, and zinc, in patients with Hashimoto's disease. Beyond their role in thyroid function, these micronutrients are crucial for immune system regulation.
Moreover, vitamin D supplementation has proven beneficial in Hashimoto’s thyroiditis and other inflammatory diseases.
Researchers applied advanced diagnostic methods known as
Metabolomic Analysis. These analysis measures tiny molecules (metabolites) and detect subtle changes in an individual's metabolic profile, often missed by standard laboratory tests.
The study employed metabolomic analysis to compare specific metabolites in urine and blood samples of Hashimoto’s thyroiditis patients with those of healthy individuals.
The findings revealed a distinct metabolic signature, suggesting that metabolic dysfunctions closely relate to the progression and severity of Hashimoto's thyroiditis.
The results open new avenues for personalized and effective treatments. Addressing metabolic imbalances through medical interventions with supplementation and dietary adjustments significantly improves patients' quality of life and reduces the risk of developing additional autoimmune diseases.
This research emphasizes the necessity for a comprehensive approach to managing Hashimoto’s thyroiditis, which, beyond medication, focuses on correcting the metabolic and nutritional factors that triggered the disease and often remain undiagnosed, negatively impacting patients' long-term health.
The Study

Identifying the metabolic profile of Hashimoto’s thyroiditis from the METHAP clinical study.
Evangelia Sarandi, Dimitris Tsoukalas, Gottfried Rudofsky, Vassileios Fragoulakis, Charis Liapi, Efstathia Paramera, Evangelos Papakonstantinou, Sabine Krueger Krasagakis & Aristidis Tsatsakis.
Nature Scientific Reports 2025.
https://www.nature.com/articles/s41598-025-89600-1

/new%20patient%20start.png)